Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | RSS
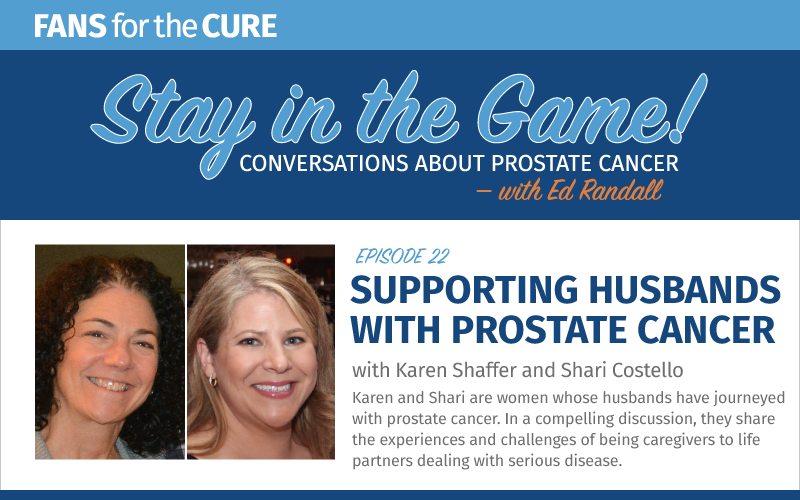
Karen and Shari are women (and good friends) whose husbands have journeyed with prostate cancer. In this compelling discussion, they share the experiences and challenges of being caregivers to life partners dealing with serious disease.
Program Notes

The Stay in the Game podcast is sponsored by Cancer Health – online at cancerhealth.com.
Cancer Health empowers people living with prostate cancer and other cancers to actively manage and advocate for their care and improve their overall health. Launched in 2017, cancerhealth.com provides accessible information about treatment and quality of life for people with cancer and their loved ones, along with information about cancer prevention and health policy.
Episode Transcript
Announcer: Welcome to Stay in the Game, conversations about prostate cancer with Ed Randall. Here we’ll chat with doctors, researchers, medical professionals, survivors, and others to share and connect. This show was produced and shared by Fans For the Cure, a nonprofit dedicated to serving men on their journeys through prostate cancer.
The Stay in the Game podcast is sponsored by Cancer Health — online at cancerhealth.com. Cancer Health empowers people living with prostate cancer and other cancers to actively manage and advocate for their care and improve their overall health. Launched in 2017, cancerhealth.com provides accessible information about treatment and quality of life for people with cancer and their loved ones, along with information about cancer prevention and health policy.
Karen Shaffer: Welcome to the Stay in the Game podcast. I’m Karen Shaffer, sitting in this month for the regular host, founder, and chief advocacy officer of Fans for the Cure, Ed Randall. I facilitate the Fans for the Cure Online Women’s Support Group, which we started in December 2020. Since then, we’ve had numerous informative speakers and valuable conversations.
My journey with prostate cancer started quite a while ago, back in August 2004, when my husband, John, was diagnosed at a young age with the disease. He was initially diagnosed at stage four. And while he was able to get many good years in after diagnosis, he passed in October 2014. I became involved with Fans for the Cure to honor John. And was invited to speak at the Cures Gala in 2017, as well as throwing the first pitch at a baseball game during one of the Cures promotional nights.
Today we’re going to have an honest discussion about the challenges facing spouses and life partners of men diagnosed with prostate cancer. I welcome my friend and fellow women’s group member, Shari Costello, for this discussion. Shari’s husband, Kevin, was diagnosed in 2014 and today is eight years down the road of survivorship. Shari, welcome to the podcast and thank you for joining me in this important discussion.
Shari Costello: Hi Karen, thanks so much for having me today.
Karen Shaffer: We’re going to begin by… at the beginning, talking about diagnosis and becoming a caregiver for a man with prostate cancer. One of the things that I wanted to talk about from the beginning is making medical decisions. Shari, you and I have talked about this before, making medical decisions from the very beginning, from diagnosis, making them together as a couple, how we navigate that, and how… Would you talk about that a little bit, how you and Kevin navigated those medical decisions?
Shari Costello: Absolutely. You know, it’s so interesting because the experiences I’ve had with family members when they were ill of my parents took care of their parents, I took care of my children. I had never had this where such a close partner had been diagnosed with something so significant. And really it shook us both. We were taken by quite surprise with the diagnosis.
I think innately we want to tell our spouse what to do. “This is these are the steps. This is where you need to go. This is what we’re going to do together. Make a plan.” That’s my way of handling situations. I want to make a list. I want to have questions. I want to see all of the best doctors.
For my husband, I needed to take a deep breath, a step back and let him really come to terms with what he was being told and make a plan for what made the most sense long term for himself. We didn’t always agree on that, you know. How I would have handled a diagnosis like his versus what he chose at the pace at which he chose to do things, that was different. And it’s a hard thing to handle but that’s how partnership goes. You know, you have to have a little give and take and you have to understand and advocate for what people need and give suggestions and strategies. But he certainly couldn’t take my opinion and my advice and use that to replace his own.
Karen Shaffer: I had the same thing with my husband, John. He handled it in a very different way than I would have handled it. You know, I’m one of those people who always religiously and methodically goes for my appointments, and he didn’t. He hadn’t been to the doctor for a complete exam in many, many years when he was diagnosed.
Shari Costello: And honestly, one of the big setbacks with COVID has been that for a lot of people today.
Karen Shaffer: Yes.
Shari Costello: They’ve been avoiding a lot of visits to the doctor or haven’t had access. So that’s a really important thing to remember right now.
Karen Shaffer: But when he was diagnosed, like you said, he took a much slower pace. His doctor insisted that he have the surgery very quickly after diagnosis, after his biopsy. But then after that, it was this, “Yeah, I’ve got to do it in my own time. I’ve got to go to the doctor’s appointment on my own. I’ve got to do this on my own to process it.” And it was hard. I felt some anxiety. I don’t know if you felt that kind of anxiety.
Shari Costello: So we had an opposite problem. My husband, from the moment he heard he had cancer, wanted to get it out of his body. He literally had his surgery… The prostatectomy was eight weeks to the day from the moment his biopsy had been done. He could not wait any longer. He couldn’t sleep during that time, he was so bothered by it. Where me, I would have wanted to step back, slow down, especially considering his age, see what other treatment options made sense.
But he was very confident about his decision. He was very happy with his decision. I had asked him before if he would have done anything differently. He has expressed that he would not. That this was what he needed to do at his age, get it out and be done with it. Of course, it’s not as simple as that. There are consequences of removing such an important organ from your body. But he is healthy, he is well, he is a survivor. And that was his only objective.
Karen Shaffer: One of the things that I had wanted John to do was go to a Sloan-Kettering or go to Fox Chase. And he was very comfortable with the decisions that he made to stay locally at the Cancer Institute of New Jersey. That’s something that has always left me a little uncomfortable. I know we talked about that a little bit last night, and I just thought if you wanted to elaborate on that and that whole process, because you did go.
Shari Costello: Kevin’s first initial diagnosis was with a local urologist here, not only a few miles from our home, he was… I really am grateful for him for discovering. His general practitioner doctor discovered that his PSA numbers were not looking the way that they should, encouraged him to pursue a specialist. That took some time, I’ll be honest because everybody thinks they’re really fine and this number doesn’t mean a lot, you know. But his doctor persisted and I persisted.
And he did go to a specialist who felt there was a problem, and, you know, after an exam in the office determined that a biopsy needed to be done. He did discover, through that biopsy, cancer. They actually are only able to biopsy… I call it like… it’s like the moon. They can’t get to the dark side of the moon. There’s the back end they can’t hit, but they hit four quadrants in the front, and three of those four quadrants had cancer. So, you know, we were very fortunate that this doctor decided to move forward and do a biopsy.
But this is the type of thing with such a serious diagnosis that you don’t go to only one doctor. You speak to other people. Whether you use that first doctor or not, you have to get a second opinion. You have to get those test results looked at by someone else and research who’s going to do your surgery.
We have some wonderful university hospitals near us, he wanted to go there. And I said, “People travel from all over the world to see the doctors at Sloan-Kettering, and we live, you know, within an hour drive us there. That’s where we’re going to go. Whether you use them or not, we are going to speak to the doctors in that facility. We’re going to hear and learn from them things that we may not have thought of or understood before.” And we did that. We did that. And we saw an additional top-rated surgeon in the city.
I was very grateful for those opportunities without having to put our family, you know, in financial hardship to travel across the country to see the top doctors in this field. So I insisted that he do that. He was not 100% sure he wanted to. Ultimately, it turned out to be a very good decision for him.
Karen Shaffer: Excellent. That kind of leads us into we talked about the surgery a little bit in the beginning, the diagnosis, and making these decisions together, which brings us to that post-surgery and actually becoming the caregiver. Because, you know, when you’re the caregiver of a man with prostate cancer, it’s not that traditional caregiver image.
That image that comes up in somebody’s mind when you say, “My spouse has cancer,” they immediately think, “Oh, there’s this frail cancer patient who’s, you know, going through chemo, who’s sick all the time that can’t work. You have to take care of them. You have to feed them, you know, help them with all their daily life tasks.” And that’s not the way it works quite frequently with prostate cancer. You know, there’s that “well he looks perfectly normal.
So I’d like to talk about that a little bit, that untraditional caregiver role and what that involves, because there are other things that a caregiver to a prostate cancer survivor has to provide.
Shari Costello: You know, I’m sitting here as we discuss this and I’m thinking to myself, perception is reality. And I wonder based on my perception of how things were prior to his diagnosis, pre-surgery and post-surgery, if Kevin would be sitting next to me right now and saying, “You know, oh, I don’t remember it that way” or whatnot.
But when it came to his post-surgery needs, it was a lot of emotional needs. It was a lot of emotional needs. Once we left the hospital, they didn’t release him until he was able to walk on his own and manage his own medications and his own care. He was uncomfortable, he was obviously unhappy, but he was able to take care of himself for the most part.
It was more about those emotional needs and the worries and the fears that come with recovery and margins and wondering, you know, about spread and if the surgeon was able to do what he promised and nerve sparing and preventing just one little cancer cell from getting out and winding up with a PSA number after your prostate is gone that says you still have signs of that there. So that was really it.
What I remember most… Although one week out of surgery, he had to go back to the city to see his doctor, and that’s when he would get checked and they’d removed the catheter and we had a huge storm. Huge. School was closed that day. Nobody was supposed to be driving. I didn’t want to get on the road, and there was no way my husband was not getting into the city that day to see the doctor.
And I remember I was… and I’m not afraid to drive. I went to school in upstate New York. I know those mountain roads. I have a truck. But the roads were not good. And I took him into the city, I drove him and made sure that he got there that day. It was taxing. It was hard. So, you know, there is some of that kind of physical stuff. But most of it is just emotional.
I have all that anxiety. I had all those worries too. So not letting that make him feel more worried was my biggest struggle during that initial time. If there had been some significant nerve damage or if there had been some additional cancer later, you know, those worries, I just had to stay positive and, you know, we’ll get through this, and I love you, and our marriage and relationship is about our children and our family and so much more. You know, keeping that hope and those good things out there were really my role as the caregiver post-surgery.
Karen Shaffer: Yeah, absolutely. I remember two things. I remember John saying to me… I said to him, “What can I do for you? What do you need from me?” And he said to me, “I need you to keep it normal.” Because we also had small children at the time. And he said, “I need you to keep it normal.” He said, “I’ll deal with the cancer, you keep it normal.” And I said to him, “That means I’m going to yell at you for socks on the floor.” And he said, “Absolutely.” He said, “That’s your role.” He said, “The more you do that, the more you keep it normal, the better I’ll feel.” He said, “I don’t want to be treated like a cancer patient. I want to be treated like your husband who’s living with cancer as opposed to your husband the cancer patient.”
Shari Costello: It’s a big distinction.
Karen Shaffer: It is a big distinction. That was something that I didn’t expect. I didn’t expect how healthy, once he recovered from the surgery, how healthy he was going to look and he was going to be physically. You know, he still built his little retaining wall in the backyard and did his gardening and did all his things. So that part of it, I guess, I was struck more like you by the amount of emotional support because of the delicacy of the type of cancer.
Shari Costello: You reminded me in what you just said, because there were so many things that Kevin was thinking about and going through that he didn’t fully express to me, so I didn’t know. And as a caregiver, I couldn’t be expected to read his mind. I remember the first trip we took in the car, driving about an hour, an hour and a half away beyond the city, and the worry that he had about if we got stuck in traffic and he needed a restroom.
Because, you know, he fortunately had very good control following the surgery but he had a lot of fears and a lot of worries. And it took some time to feel back to normal in those ways. I didn’t know on that drive that he was concerned about that. So we’re driving along and we’re talking about something, and he just wasn’t being himself. And I said, “What is the matter with you? We’re going on this nice trip. We’re having this great time.”
And you know, that was the first thing he said, “well, I need the bathroom and I don’t know where I’m going to stop. We’re out here on the highway and there’s no rest area for another 50 miles.” I said, “All right.” But it didn’t occur to me. I didn’t understand it because he was so healthy on the outside, because everything that he did for all of those months and months and months following surgery, he seemed totally fine but all of that was still there. And that was an aha moment for me, trying to remember.
Karen Shaffer: And that was something that we had difficulty with with extended family and friends. You know, one of the things that we kept getting was, “What’s your problem? You look fine. What’s your problem? What are you complaining about? Why are you going back to the doctor? You look fine. Everything’s fine.” But in there, it really wasn’t. There were so many worries. There were so many concerns. And like I said, because of the delicacy of the type of cancer and how it affects men and how it affects their self-esteem and their feelings about themselves and their manliness and their men manhood, these are things that men have difficulty expressing.
Shari Costello: My husband, he Googled, “You know, can things get smaller if you remove your prostate.” There are those worries. The same way I would worry if I had breast cancer and I was going to have to have a mastectomy. You lose your feelings. There’s a lot of things connected with that. And it’s hard to put yourself in that position if you’re like, Men always think about their genitals. And this really just made the focus all about them.
Karen Shaffer: Right. Exactly. I think it’s something that they had so much trouble talking about and almost expect us to read their minds about. But we have no experience with not having those genitals that we as caregivers, you know, we kind of grasp at straws trying to figure out how to make them feel better. How am I going to make this better and how am I going to make this right?
Shari Costello: The best connection I’ve been able to make for myself about this is postpartum. You know, after a baby is born, women feel their bodies are so different and you struggle with a lot of the same types of possible incontinence and feeling and all of that stuff that, you know, if you had stitches or different things, could impact your sensations. Well, it’s interesting because women have babies every single day and you have multiple babies. But it’s really the closest that I could come to making a connection to what he was experiencing.
And here I am, you know, it still impacts him today, and yet my children, the birth of them is like a very distant memory. So even though he’s healthy and well, those fears still linger. Every six months when he goes for his PSA test and, you know, many, many times when we think about what we’ll do on our weekend and if we’re going out of town together, an intimate scene and long trips.
Even things like exercise. You know, my husband used to be an avid runner and he enjoyed it. And he still runs. But I think that without him saying so, I have come to believe that maybe he’s concerned about the connection of incontinence and running. Although he does a great job with all of it, it’s been very fortunate, I think it’s just a worry that lingers. And as the caregiver I try really hard to remember that. Eight years down the road, it’s easy to not remember. But not for him. It’s something I think he thinks about every day.
Karen Shaffer: Right. And because of what’s in our wheelhouse in our experience, that postpartum a year later, if you’re over it.
Shari Costello: You’re having another.
Karen Shaffer: That’s right. You’re thinking about having another.
Shari Costello: That’s right.
Karen Shaffer: But thinking about that whole “he looks so good, he looks so healthy,” and then talking about finding support for yourself from friends and family and people who can understand why you need that support, I found it difficult to talk to my friends and family because a lot of them would look at him and say, “But he’s fine. What are you worried about?” “Well, we’re worried the cell might have escaped, his PSA went up a little bit.” “Well, look at him. He looks fine. What are you worried about?” And they couldn’t seem to… So I found very little support out there.
Shari Costello: I’m sorry for that. That’s really hard. It’s hard to be a mom, to be a wife, to be a caregiver, and to not know where to go to get what you need because the only way you could support John was by having a sounding board and somebody that you could talk to so you could vent and let that go a little bit before you came back home to him.
Karen Shaffer: Exactly. And where have you found support?
Shari Costello: Oh, you know, I have to say that nobody around me was really familiar with prostate cancer in the way that it was going to impact my life with such a young husband and a young family. Everybody had heard of it. Everybody knew a grandpa who had it or knew a father that was diagnosed with some sort of problem. But nobody had any experience going through what I had gone through.
So I don’t know if I really relied on family and friends for that type of support and information. I was fortunate that the Internet really had a lot of good information available. That I could go on, you know, really useful websites, which now Fans for the Cure, would be a great place to go and start. You mentioned a site last night, and we’ve had some that we’ve discussed through our groups that have so much good real information. But I think Healthline was a place that I went and stuff like that.
But I guess I didn’t feel alone, but I didn’t have anybody that I could talk to about it. Even until our group eight years, seven years down the road after surgery, it took that long. And I think that’s why I got so emotional at times in our group, because it was the first time I ever really expressed so many of my own worries and so many of the consequences.
Karen Shaffer: So you were isolated also in that?
Shari Costello: Without knowing it, I was.
Karen Shaffer: Right. I’m not saying that my friends and my family weren’t supportive. They were as supportive as they could be with what they understood. There was a lot of misunderstanding because of lack of experience with prostate cancer. Nobody else in my family or any of my friends have had spouses or themselves have had prostate cancer.
Since John’s passing a couple of, you know, as my friend group is getting a little older, some of my friends have had some elevated PSAs but it’s been just a watchful waiting. And they’re starting to say, “Now I understand. Now I understand.” But at that time, there really wasn’t much understanding. I’m glad we could be that support for you, Shari.
Shari Costello: Yeah, thank you. It’s really been a wonderful group.
Karen Shaffer: So in all of this, thinking about our families and thinking about where you got information from and how you made these medical decisions and what you’ve been through with your husband, what would you say is or are a couple of valuable or enduring life lessons that you’ve learned as a caregiver, as a partner, or as a family where there’s prostate cancer?
Shari Costello: So the very first lesson that I’ve learned—and I haven’t learned it, I’m still working on it—is really to take a deep breath and pause. I’m a go-getter. I immediately made a list of questions for the doctor, and I made a list of different options that he would have, whether it be radiation seeds or the CyberKnife or prostatectomy, or wait and see. And I had a whole list of questions for each one. I had all of this information, and it overwhelmed Kevin. It was too much too fast for him.
And even though he knew this had to get out of his body right away, he couldn’t hear all of the things that my brain was seeing and thinking about as quickly as it was because he just kept hearing the word prostate cancer. “You have cancer. You have prostate cancer.” And thinking about, “Oh, my God, I’m 42 years old…” He was 42 years old, 41 when he was diagnosed, “And 42 I’m going to have to have my prostate removed?” It was stuck. So I had to take a deep breath. That was really important. And I try to be a better listener in a lot of areas. That was something that endured from that.
Additionally, ask as many questions as possible. These doctors have heard all the questions and yet you’re entitled to hear the answers specific to your case and your life. It doesn’t matter what you want to ask. Kevin could look at me and make a face at me at the doctor, but I’m going to ask this question because this is our opportunity to interview a doctor to learn and hear something that maybe nobody else told us. And each doctor reframed things in a way that made it clearer. So by repeating the question, by writing it all down.
I had one notebook where I kept all of our information. And every time that I learned something new or every doctor that gave me, you know, a piece of the puzzle, I put it in there. My job was to that and be able to tell that information back to Kevin because the last part of it is I couldn’t make any decisions for him. He had to make all of the decisions when it pertained to his body. He had to advocate and have informed consent about what was going to happen to him. Although we made decisions, we talked about it and I feel like we had enough conversation that I was confident and comfortable in what he decided to do, ultimately, it was his decision. And my job as caregiver was to support him no matter what happened and no matter where we wound up. And just pray. Pray.
I watched a lot of movies while he was in his surgery and recovery room. I brought just only funny movies. My brother-in-law back then, you know, you had to get little discs of things, he gave me funny movies. I watched as many funny movies as possible to try and laugh. I told my family, “Don’t come, I’m okay here. I’ll be all right.” But my sister came. She met me there and I didn’t know she was coming in. So don’t be alone.
Karen Shaffer: Absolutely.
Shari Costello: Have people around you. Making sure my children were cared for. It was the first time Kevin and I ever spent the night away from our children. At the time, I think my daughter was five and my son was nine, and we’d never been away from them for the night. So making sure that I didn’t have to worry about them and could just focus on him. That was a really important part of what we needed to do in order to make sure that this could be successful. Those were some things that I’ve learned and would definitely do again-
Karen Shaffer: Absolutely.
Shari Costello: …if I was faced with a circumstance of needing to handle health care with my husband like that.
Karen Shaffer: I did some similar things. I started the list, you know, because the first thing is, “Okay, we’ve got to take care of this. Let’s do this.” And I started my lists and John took them and I never saw them again. I never saw them. I don’t know what happened to them. I can only imagine. But I never saw them again. I tried to keep a binder of all of everything that related to his prostate cancer and his care and his doctor’s appointments. He was a little sneaky. He would make doctor’s appointments and not tell me when they were. And then he would come home and tell me what the doctor said. So he just felt more comfortable going on his own.
Shari Costello: Was he a caregiver in his personality before his diagnosis?
Karen Shaffer: Yes.
Shari Costello: Yeah. It sounds like he just kept wanting to take care of you and all you wanted to do was take care of him.
Karen Shaffer: In fact, it’s funny that you say that because my kids always commented that our arguments were always about who loved who more and who wanted to do more for that person at that particular time because the other one should go relax, you know. So that was the kind of relationship that we had. But absolutely, he really wanted to protect me and I wanted to care for him. That wound up in conflict a few times.
I would say that one of the lessons that we learned from it was how to balance that, because towards the end we finally figured it out. It took a few years but we finally figured it out. And at that point he was inviting me to come to the doctor’s appointments. Even if it was the type of situation where I couldn’t get off of school, but I could get somebody to cover one period for me and I would be on the phone and he would have me on speakerphone so at least I could hear what was going on. He started to bring me in. And he realized that by blocking me out, he was not protecting me, but he was making me more anxious.
So that’s something that we both kind… And I accepted the fact that he wanted to protect me. I stopped fighting him on that, that he wanted to protect me. But I absolutely agree. Ask as many questions as you can. Seek out as much information as you can.
That kind of takes us to something that we’ve talked about before, and that’s caring for the caregiver, caring for ourselves, fitting in self-care, nurturing the relationship with our partners. I know that we’ve talked a little bit about how you fit in self-care because you have quite the hectic schedule between work and your kids. So how do you fit in self-care? What do you do to take that little break and just make sure you’re a strong caregiver?
Shari Costello: You know, it’s really cyclical because there are some times when I’m just not taking care of myself. You get so busy taking care of everybody else. And it takes a friend like you to say, “No, you need to find that time for yourself.” Or some of the women I work with say, “What’s going on? You’re not quite yourself.” And you start to realize that you’re giving 110% to everybody and leaving nothing at the end of the day for you.
So one thing that I promised myself this year, eight years down the road after Kevin’s cancer, but also 17 years after the birth of my first child, my son, and 21 years after my getting married, I finally have given myself over this past year time. But I have to sneak it in the morning before everybody else gets up. I was going to the beach and walking right near the water, and I just love, love, love being outside and watching the sunrise and hearing the ocean. There’s something really very cathartic and healing about being in the sand and there at the beach. I joined a gym, so I’ve been doing that. I sneak in a little mani-pedi here and there.
But really my favorite thing to do is to go and have a bite of dinner with some girlfriends, you know, just an hour. I won’t drive all the way out to them and they can’t drive all the way out to me. So we’ll meet somewhere in the middle. I won’t go more than 20 minutes, so it doesn’t take up too much time. And I could still pick up some more late-night activities. But just sitting down and having a nice, enjoyable meal with some friends and laughing and getting away from the chaos of it is probably my number one thing for self-care.
Karen Shaffer: Yeah. Yeah. It’s interesting because I was in the same situation. My kids were eight and eleven when John was diagnosed. I was working also and he was working as well as, you know, having the other issues that come along with prostate cancer. Self-care at that time, you really didn’t think about it. So he would get me a massage or he would get me a gift certificate for a mani-pedi, and he would say, “Go. You can go. Just go. Go have breakfast with your friends. Go have lunch with your friends,” whatever it was. He would force me. He would force me to go.
Some of it I would feel some guilt about it because I just felt that he was dealing with so much that for me to take that time… And he said to me, “Karen, the way I take care of myself is I go out and I play in the dirt.” He loved to garden. He said, “I’m playing in the dirt. Yes, I’m making your house look beautiful, but that’s what I do for me.” He always called it playing in the dirt. “I’m going to go out and play in the dirt now.”
Karen Shaffer: How about nurturing that relationship? What do you guys do to nurture a relationship and kind of put everything else on the back burner?
Shari Costello: We’re still really learning in that area. I think couples, regardless of prostate cancer diagnosis or any other type of illness, you hit a point, with your children, where your whole life becomes about them. Everything you do is focusing on what they need and where they’re going and what their life is filled with. So we’re just now getting to a point where we took a trip together, where we spent a weekend out at a bed and breakfast. We go to dinner as often as we can. And we’ve started, you know, binge-watching some Netflix programs and things like that. We’re trying to do those things together, building those shared experiences.
But it’s a big work in progress. We’re really trying to find that healthy balance and bring it back. Because it’s so easy to get wrapped up in the day-to-day of everything that needs to get done. If I get up, I go to the gym at 6:05 in the morning, I come home by 7:05, I jump in the shower by 7:30, I’m putting Eva on the bus. By 8:00, I’m at work. That’s 2 hours in the morning, I’ve already done so much. And I may stop at the post office and grab some milk at the grocery store and then work all day and come home. And the evening goes just like that.
So you have to schedule it. You have to have a plan. It’s kind of like prepping meals. You have to prep it a little bit. Make a reservation, have a show, and have it ready to go on the fly. And without that mindfulness about it, it can slip away very, very easily.
Karen Shaffer: Absolutely. Absolutely. And then, you know, you put some of the stress and the strain of the, like I said, the delicacy of prostate cancer on top of that, and sometimes it becomes uncomfortable to nurture that relationship. It reminded John of what he couldn’t do.
Shari Costello: On the more intimate side of it, there’s definitely anxieties and worries and the impact. I wish we could talk about it more. I wish we could have more open conversations. It would help with those… It would help to build something better between us. And it’s a hard thing to talk about, you know? So I realized today we’re not diving into that side of it, but certainly the emotional peace between a couple and being able to talk about the most private, intimate things that people typically experience, or, you know, just occur so naturally is a hard thing. And that’s a conversation for sure for a whole nother time.
But as a caregiver, most of my job in that area is just to let him know that I love him. And I couldn’t be happier with where we are today with the relationship, both emotionally, socially, physically, all of those things. And the fact that, you know, we’re going to watch my son graduate next year and send him off to college and that he’ll be a part of all that is paramount beyond anything else. So I have to just keep continuing to say that that I wouldn’t choose another partner then and I certainly wouldn’t choose another partner now. I’m very happy with where we are. I hope that he can hear that from me because, you know, I know my husband and I know that he might have a hard time with that. Same way I probably would if he was sitting here saying that about me.
Karen Shaffer: Yeah, Yeah. But I’m sure he’d be smiling inside. Lastly, to wrap all this up, advice for anyone who’s just starting on this journey? What would be your big piece of advice for somebody, for a spouse, or a life partner who’s just starting on this journey with the man in her life who’s been diagnosed with prostate cancer?
Shari Costello: You know, you have to find a group of people who’ve been through it before, the wisdom of the others, and not just one person, but many like this group. Because as we’ve spoken to the other women, we have so many shared experiences and yet we also have a lot of things that were different. But we can learn so many things from each other.
If I was to be approaching this now as a newbie, which I wish I wasn’t an experienced partner with this, but if I was looking at this from the onset, I would want to have someone like you, Karen, to talk to, and I would want my husband to have someone like the Men’s Fans for the Cure group that he meets with because you can gain a lot of insight from those who’ve come before and learn some of the mistakes that people made as well as hear many of the good decisions that helped them to be survivors today.
Karen Shaffer: Shari, you always take things so beautifully.
Shari Costello: Well, thank you.
Karen Shaffer: But I can’t even thank you enough for doing this. You definitely made it a lot easier and a lot more fun to do this with you. And I thank you on behalf of our listeners who will certainly benefit from your experiences and the information that you’ve shared with us today. It’s been a pleasure. I just can’t thank you enough.
Shari Costello: Well, thank you, Karen. Your group really has been a blessing for me. I’m glad to have it. And I thank Ed for his advocacy and for, you know, the things that he’s been able to help with my husband and many of the men out there who might not have this information. So thank you to all of your Fans for the Cure. Thank you, Karen, and everyone who made today possible. I really do appreciate it.
Karen Shaffer: Thank you, Shari. So this was the Stay in the Game podcast brought to you by Fans for The Cure and the Cancer Health. I invite all women listening to this podcast to join us for the next online women’s support group meeting. Just go to fansforthecur.org to learn more, get the schedule, and register for an upcoming meeting.
Announcer: Thanks for listening to the show. You can find program notes and a full transcript at the charity’s website, fansforthecure.org. Be sure to subscribe to our podcast in iTunes, Spotify, Stitcher, and everywhere. good podcasts are available. And if you like what you heard, a positive review on iTunes will help other people also find our show.

