Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | RSS
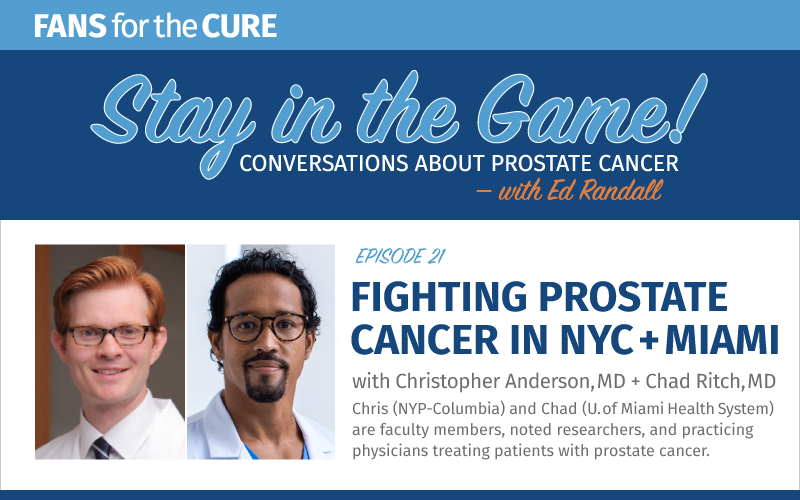
Dr. Christopher Anderson is an Assistant Professor of Urology at Columbia University Irving Medical Center, and urologist at New York-Presbyterian/Columbia University Irving Medical Center. His research includes outcomes after robotic prostatectomy, access to care for bladder cancer patients, and the study and development of active surveillance strategies for men with prostate cancer.
Dr. Chad Ritch is an Assistant Professor of Urology at the Miller School of Medicine, as well as a urologic oncologist at Sylvester Comprehensive Cancer Center, both of which are part of the University of Miami’s Health System. His research has led him to study imaging in refining prostate cancer treatment, robotic vs. open surgery approaches, and the role of race and ethnicity in prostate cancer outcomes. Dr. Ritch also has an MBA from the University of Chicago.
Program Notes
Christopher B. Anderson, MD MPH
- Christopher B. Anderson on Twitter: @cbanderson2014
- Dr. Anderson’s bio on Columbia University Irving Medical Center
- The Department of Urology at Columbia University Irving Medical Center/NewYork-Presbyterian Hospital on Twitter: @columbiaurology
- Herbert Irving Comprehensive Cancer Center on Twitter: @columbiacancer
Chad Ritch, MD MBA
- Chad Ritch on Twitter: @chadritchmd
- Dr. Ritch’s bio on University of Miami Health System
- University of Miami Health System on Twitter: @umiamihealth
- University of Miami’s Miller School of Medicine on Twitter: @umiamimedicine

The Stay in the Game podcast is sponsored by Cancer Health – online at cancerhealth.com.
Cancer Health empowers people living with prostate cancer and other cancers to actively manage and advocate for their care and improve their overall health. Launched in 2017, cancerhealth.com provides accessible information about treatment and quality of life for people with cancer and their loved ones, along with information about cancer prevention and health policy.
Episode Transcript
Ed Randall: Hi again everybody and welcome once again to the Stay in the Game Podcast. I’m Ed Randall, the Founder and Chief Advocacy Officer of Fans for the Cure.
I’m so fortunate to have two of the country’s most renowned urologists, surgeons, teachers, researchers, and public policy advocates with me today.
Dr. Christopher Anderson is an Assistant Professor of Urology at Columbia University Irving Medical Center, as well as a urologist at New York Presbyterian Columbia University Irving Medical Center, where he performs both open and robotic surgeries, including robotic prostatectomy for the treatment of prostate cancer.
His research has included outcomes after robotic prostatectomy, access to care for bladder cancer patients in the study, and development of active surveillance strategies for men with prostate cancer. He completed his urologic oncology fellowship at Memorial Sloan Kettering Cancer Center and has also earned a Master of Public Health degree from Harvard University. And most importantly, he has lived long enough to see his beloved Chicago Cubs win the World Series.
Joining Chris is Dr. Chad Ritch, who is an Assistant Professor of Urology at the Miller School of Medicine, as well as a Urologic Oncologist at Sylvester Comprehensive Cancer Center, both of which are part of the University of Miami’s Health System. Last March, he was elected to a three-year term to represent the Society of Urologic Oncology as a member of the prestigious Commission on Cancer.
His research has led him to study imaging in refining prostate cancer treatment, robotic versus open surgery approaches, and the role of race and ethnicity in prostate cancer outcomes. And like Dr. Anderson, Chad also needs LinkedIn premium to list all of his credentials. He also has an MBA from the University of Chicago. Welcome to you, Dr. Ritch.
There was a coin toss today prior to today’s podcast won by Dr. Chris Anderson who decided to defer. So Dr. Ritch, again, we welcome you to the Stay in the Game Podcast. At this point in your career, what do you find to be the most compelling part of what you do? Teacher, researcher, or physician who sees patients?
Dr. Chad Ritch: Let me say thank you for having me. It’s an honor to be around esteemed company like yourself and Dr. Anderson. So in terms of question, “what’s the most compelling?” it’s a hard question to answer. But I guess the thing that keeps me waking up every morning and coming to work are my patients. I really enjoy seeing patients and taking care of them.
The other two things, the teaching, and the research, it kind of falls into place afterwards. Because when you take care of patients, you really want to improve their outcomes and know that you’re doing the best thing for them. And the best way to do that is to do research into what you’re doing and how you’re treating patients to see if you can improve on that. So, you know, the taking care of patients comes first, and then the research sort of falls into place afterwards.
And then the teaching side, I really enjoy. But you know, what that really translates to is it’s an extension of what you can offer to your patients. Because in medicine we have this thing where you say: see one, do one, teach one. And really what you’re saying is basically you can extend your skill set to other people, and then they go on to treat other patients. So really it starts with taking care of patients and then the other things, research, teaching, kind of falls into line with it.
Ed Randall: And Chris is another physician with three paragraph job description. I’ll form the same question for you. At this point in your career, what part of your workday or workweek presents you with the type of challenges that keep you coming back for more?
Dr. Christopher Anderson: Thanks so much for the question, Ed. It’s really great to be here with you and good to see everyone’s face. I think Dr. Ritch and I are kind of at similar point in our career, relatively early on. We’ve been in practice for, you know, six, seven years, I’d say.
The thing that keeps me coming back are the people. Just like Chad said, our patients, our co-workers, our colleagues, you know, the people we work with every day are really what makes any job fulfilling. And our job is really no different.
The particular challenges that keep me coming back for more certainly are the clinical challenges that we see every day in clinic, patients are referred in with difficult problems, with unique circumstances that really require a little extra brainpower and maybe a little more teamwork to try to manage.
And also the teaching. I think that our resident involvement in our cases in our patient care is incredibly important as it is important for us to teach them what we know and try to help them become doctors who can take care of us one day. So I think that’s an incredibly fulfilling part of my job that certainly keeps them coming back for more.
Ed Randall: Both of you perform and teach robotic prostatectomies as well as carrying out research on approaches and outcomes, including comparisons with open surgery. Men often attend our support groups as they are in the process of making a treatment decision or in the case of a prostatectomy, whether it will be robotic or open surgery.
Their complaint is that the robotic specialists oversell the robot, while for the open surgery urologist, there’s no substitute for his or her hands. Based on your experience in research, can the two of you please provide us with an objective perspective on the two approaches to prostatectomy surgery? Chad, you first.
Dr. Chad Ritch: You know, that’s sort of an age-old debate that’s been going on since the robot came around. And I think what it boils down to is, you know, it’s not so much about the instrument or tool you’re using, whether it’s robot or open surgery, it’s about the surgeon and their experience. And that’s what all the evidence that when we, you know, do research in the medical literature and look for what’s the difference, it really boils down to the surgeon and their experience.
People who have a lot of experience doing surgery, whether it’s open or a robot, have the best outcomes. The robot isn’t going to take a surgeon who is not as experienced in doing a procedure and make them better. But it is a fine tool for marketing and advertising. And unfortunately, I think a lot of healthcare systems have kind of overplayed their hand and use things like the robot to attract patients. But truthfully, it’s a surgeon and the surgeon’s experience that makes a difference.
And when you look at objective data about outcomes for robotic versus open surgery, if you have a very experienced open surgeon, very experienced robotic surgeon, there really is no big difference as far as how the cancer control is. The big difference lies in the blood loss and the recovery.
So the one thing that has definitely changed with the robot and improved is patients can go home the next day after surgery almost always. And even in some cases now people are doing outpatient robotic prostatectomies. And then the other thing is the pain control. So you almost never have to give anyone you know, opioid pain medications.
Whereas with open surgery, probably you’re more likely to have to give them some sort of opioid pain medication, and their recovery may take a little bit longer. That’s probably the main difference.
Dr. Christopher Anderson: I completely agree. I think that a radical prostatectomy is the operation. And how you accomplish that is really up to the skill of the surgeon. An open and robotic approach are equally effective. There are some merits to one over the other.
Really the best study that looked at this, there was a study that randomly assigned patients to open and robotic surgeries published five years ago out of Australia. And you know, the two arms did pretty much the same when you looked at them over time. Their function was very similar, their cancer control rates were similar, the complications were similar.
Similar to what was Chad was saying, it’s not a substantial difference in long-term outcomes. Now, yes, the open surgery group had more blood loss, and there may be some other short-term differences, but overall, it’s a similar operation when performed open robotically.
I agree that there are merits to the robotic approach that are advantageous for patients: that the recovery may be a little bit easier, the hospital stay a bit shorter. And that’s why at least 95% of all prostatectomies in this country are now performed robotically.
Now, that’s partially market-driven and there’s some good objective data to support that change. But I wouldn’t let anyone be fooled nor do I try to fool anybody by selling them on a surgery that is a panacea. You know, that this is the perfect surgery because we’re using a robot. You don’t have to worry about anything. The counseling is the same regardless and the outcomes are the same regardless.
Ed Randall: If there’s been one consistent complaint from men in our support groups, it’s been that their doctors soft peddled the side effects treatment that have resulted in impotence and incontinence, which are life-changing and life-limiting realities. Or maybe the doctors spoke the words but the men only heard what they wanted to hear.
As patient advocates, how does Fans for the Cure get the word out to doctors that men can handle the truth where we heard that before? Chris, I’ll start with you.
Dr. Christopher Anderson: Right. So this is really important. And this is what I spend a lot of time doing in clinic, I’m sure Chad does as well, which is talking to men for, you know, 45, 60 minutes on end about exactly what to expect with this operation. Because one of the key factors in making sure that patients do well is setting the right expectations. And frankly, that doesn’t always happen.
So, one piece of advice is that if you’re considering having a prostatectomy, you should really be seen by someone who does a lot of these surgeries, who’s familiar with them and good at them, and can counsel you accurately.
It’s also okay to ask questions, which include questions about: tell me about how your own patients do? What is your own data look like? Or can you tell me about what’s been published? What do other people report as far as expected continence rates and potency rates? Those are totally fair questions that anybody who is an expert in prostate cancer surgery should be very familiar with.
Ed Randall: Chad, your thoughts?
Dr. Chad Ritch: I agree. Continence is really important, and taking the time to not only just consultations but understand their expectations. So it’s always important to me. I usually start off the conversation with asking men, “Well, tell me about your erections and your sex life. How active are you?” So that sort of sets the bar for how I come to them and explain to them that, yeah, there’s going to be a change in your quality of life potentially, because you are very sexually active.
Or somebody says, oh, you know, they’re not that sexually active, maybe that side of things, isn’t that significant for them. So it’s important to understand the patients, where they’re coming from, and what their priorities are.
And then honestly, you know, I try not to sugarcoat it. And I tell a lot of patients that when I speak to them about the side effects, it’s going to sound like those TV commercials where there’s a new drug, and they say, “Side effects may include…” and then they list off about 50 things and everybody blacked out.
And I tell them, “I’m going to tell you a couple of side effects. Stop me, ask me questions.” And then we pick up from there. So I think the main thing is just to be honest about outcomes and experience.
Ed Randall: Dr. Ritch, let me stay with you. Here’s a quote from you on the miR Scientific website. “Prostate cancer screening is vitally important to men who are at high risk of harboring an aggressive disease that might lead to death.”
As a member of the Commission on Cancer and other organizations and committees that determined policy, can you please reconcile for us the recommendations of the US Preventive Services Task Force with the poor outcomes and increases in late stage disease when screening numbers decline, as they have, since the initial USPSTF recommendation in 2012?
Dr. Chad Ritch: So, as people listening may already be aware, back in 2012, the USPSTF, Preventive Services Task Force, gave prostate cancer screening a grade D recommendation. Basically said it was a bad test for screening for prostate cancer.
A lot of that was driven by generations of bad practices and data where basically anybody who had a PSA that was quote-unquote, “abnormal” got a biopsy and essentially got treated. And there was a less nuanced approach than there is today with how we treat prostate cancer.
And because of that grade D recommendation and the press around it, you know, several studies were done, which basically showed in subsequent years the rate of screening did decline. And then even some studies they show that the presentation of the disease, prostate cancer, was at later stages for some cohorts.
So it was almost like a complete string in the pendulum away from doing anything and kind of just saying, you know, “Talk to your doctor, don’t worry about getting screened.” And that’s the message that a lot of people got, even primary care doctors.
So in doing so, they also potentially harm people who had a family history of prostate cancer because they weren’t sure what to do, whether they should be getting screened. Black men were potentially being harmed because they didn’t really say much about whether black men should be screened versus general population.
Again, there was a body of literature or there is a body of literature emerging that show that more men are presenting with later stage disease in the screening is being done.
But I think, on the flip side, the positive that came out of it is that it forced a lot of urologists in practice and researchers to look harder into how we can screen smarter. And instead of saying, no screening, basically figure out what’s the population most at risk, what are the tools we can use in those patients. And a lot of this is now driving the research that we see today.
So you mentioned like neuroscientific, you know, that they’re exploring using a new test, an exosome test, a biomarker in the urine to see if we can screen men better and avoid doing unnecessary biopsies. And other different types of technology are coming out this way because of USPSTF putting urologists on notice for PSA screening practices.
Ed Randall: Chris, anything to add?
Dr. Christopher Anderson: Yeah, I completely agree. The Taskforce recommendation a couple years back was a wakeup call for us all. And I think it was shining a light on the fact that there were some problems in the way we were screening and treating men for prostate cancer. And this was kind of a nice way for us to correct that.
It was a slap in the face in many ways but I think it’s led to a lot of great changes. So, as Chad said, now I think we’re much smarter about who we screen, how we screen them, how we select patients for invasive testing, such as prostate biopsy.
We’re no longer just willy nilly biopsying every man that walks in the door. We’re trying to be much more thoughtful about, you know, who is it particularly high risk of a potentially lethal prostate cancer, who would benefit from that diagnosis and benefit from that treatment? You know, those are the guys we want to find. Those are the guys who want to biopsy.
In addition to the biopsy questions, it’s also, you know, we’re getting much better about identifying who needs to be treated aggressively and maybe who does not. Over the last 20 years, the use of active surveillance has really taken off in this country. That’s one of the reasons why the recommendations have switched back. And they’re not so much against screening anymore because we’re not taking everyone’s prostate out and radiating everyone’s prostate.
Now we’re being very thoughtful about identifying men who are at low risk for prostate cancer death and spread. And we are offering surveillance to them, which is a careful monitoring, but it avoids a lot of the side effects associated with aggressive treatments.
So, the smarter screening, more thoughtful selection for biopsies and more thoughtful selection for aggressive treatment I think is all led to meaningful changes in how we evaluate men at risk for and who have prostate cancer.
Ed Randall: Dr. Ritch, we are currently working with the former Chicago Cubs, the Hall of Famer, and community leader, Andre Dawson to establish local programs to increase prostate cancer awareness in screenings and reduce health disparities among black men in Miami-Dade County.
To be clear, Florida’s prostate cancer numbers are among the country’s best. But black and poor Latino communities in Miami-Dade County are among the worst for screenings, diagnoses, and outcomes. As somebody who studies racial disparities as part of your research and as someone more than familiar with the Miami-Dade health landscape, what form would you recommend that our awareness and screening programs take?
Dr. Chad Ritch: That’s an important point. In fact, I totally agree with you. And anecdotally, in my practice, I can see that black or Hispanic communities are the ones that seem to be harmed a lot by not having enough access to care or not having good advocacy.
Honestly, I think a big part of it is community outreach and engagement. And what’s unique to South Florida is that we have a large black population, for example, but it’s so diverse in the sense that there’s Jamaican, Bahamian, Haitian, Caribbean culture plus US black.
So a lot of the screening programs need to be sort of a little bit more culturally aligned. Because even though the black population in general needs to be screened because of prostate cancer risk, these programs need to consider “Am I going into a Haitian community, and how can I engage our community? Am I going into a predominantly Jamaican community? How can I engage our community?”
So the Sylvester Comprehensive Cancer Center where I work has a community engagement program, well, they kind of do that. And they look at not just the population as a whole, but specific cultural programs that may be more in tune to some of the other cultures that are within the black community.
And then another thing is just having, just like with Andre Dawson, is having community leaders and advocates who can not only go into these populations, but also be representative of these populations, talk about their experience.
And then on top of that, the next step is having representation at the physician level. So having minority physicians who treat prostate cancer going out into the community, speaking with them, and engaging them is another great way that I think we’d be more successful in getting black and Hispanic population to be screened.
Just as an anecdotal story, I am from Jamaica originally. They have this big… I don’t know if you guys eat jerk chicken, but they have this big thing called the Jamaican Jerk Festival in South Florida. And the last time I went there pre-COVID, I was surprised because there wasn’t any healthcare booth or awareness from any health system in South Florida, and we have quite a few.
And I was like, “This is an opportune time to be promoting prostate cancer awareness and screening, but there’s nothing there.” So there’s still work that needs to be done in a lot of these community events to engage the population and improve awareness and screening.
Ed Randall: Chris, let me stay in that theme. Black men nationally are twice as likely to die after receiving a prostate cancer diagnosis than white men. We all know about disparities in identifiable risk factors, environmental risk factors, underrepresentation in clinical trials, and lack of access to quality health care.
Doctors on this podcast have cited studies showing genomic differences in black men’s tumors. Chris, help us think outside the box for a moment. What are the kinds of things a charity like ours can do to start reversing these stark outcomes?
Dr. Christopher Anderson: Right. I think there’s some simple things that can make a big difference. So as you pointed out, men of African descent in this country are at increased risk of prostate cancer. They are consistently identified as a higher risk group. They should be screened regularly and probably at possibly a slightly younger age than white men.
So, you know, getting the word out about the importance of screening among black men I think is vitally important. What’s the best way to do that? Well, I think there’s probably many ways to do that. Starting in communities, primary care doctors, local support groups, etc. So there’s no simple solution to how to get the message out. But it has to be done probably multiple different ways.
The other important thing is access to care. There’s some interesting data that’s come out over the past couple of years about men treated in the VA Health Care System. So veterans treated at the VA Health Care System have equal access to health care. There’s no insurance issues, everyone gets the same care.
And what they found is that when you compare the outcomes of black and white men in the VA system, they actually do reasonably well. I mean, they both have similar outcomes when treated for prostate cancer. So if you take the access factor out of the equation, you know, maybe our outcomes are actually more similar than they are right now. And so if we can get men similar access to expert prostate cancer care, I think that can also make a major difference among black men.
Ed Randall: Chad, for a moment, let’s talk about the improvements in the short and long-term pipelines for diagnosing prostate cancer, identifying the most aggressive cases and treatment protocols to both extend lives and minimize life-changing side effects.
Dr. Chad Ritch: There are companies that are working on things like improved diagnostics to screen patients and avoid unnecessary biopsies. We talked about one in the neuroscientific. There’s other blood tests, you know, that can help if you’ve had a negative biopsy and you want to see if you need to do a re-biopsy. So there are companies that are working on good diagnostic and screening tools in the setting of an elevated abnormal PSA to avoid unnecessary biopsies.
And then there are things like better imaging. Prostate MRI has been something that has really exploded in the last, I would say, 10 years. And we really improved our ability to find suspicious areas in the prostate and figure out who needs to get biopsy. And even in recurrent cases, after things like radiation, there may be some utility there.
And then there is, even at later stages, new imaging techniques called PET scanning. And there’s a specific marker PSMA, Prostate-Specific Membrane Antigen, that can be used in a PET scanner to find prostate cancer at very, very low levels of PSA. So in men who have been treated and their PSA may be going up, we can actually detect it better using this test that is more sensitive.
And even taking it to the next step, when you talk about treating aggressive cases, they found ways to link PSMA with a molecule that can actually treat the cancer radially, the molecule that can treat the cancer. So it finds it and treats it at the same time.
So that’s something that we may see more of in the future. So when you talk about long term, we could actually be seeing a lot of these advanced cases getting quote-unquote, “cured” by some of these advanced diagnostics like PET and PSMA driven modalities.
And then the last thing I just wanted to touch on which is also becoming sort of a hot topic is Focal therapy. So very early stage cases, we think about cancer treatment as being radical. It’s called a radical prostatectomy. But some men may not need a radical prostatectomy. They may be able to have focal therapy just pinpointed to the area when these new diagnostic imaging modalities can show us where it is, we can just treat that area. And that could be something we see more of in the future as well.
Ed Randall: And Chris, what are you seeing down the road in terms of diagnoses and treatment? When Fans for the Cure rolls out its mobile testing unit in 2023, will the PSA blood test still be the centerpiece of prostate cancer screenings?
Dr. Christopher Anderson: Yes. To answer your second question, yes. PSA is still the best and only recommended test to screen for prostate cancer. As we talked about before, I think we’re getting better at using PSA and identifying men who should and more importantly shouldn’t be screened for prostate cancer.
If you’re very, very young with no risk factors or if you’re very, very old, you’re probably not a good candidate for screening. And that’s something that we’re trying to do a better job of to avoid unnecessary testing and also unnecessary treatment.
Now, as far as what’s coming down the road for diagnosis and treatment, you know, Chad hit on a lot of the high points. I think we’re getting better at staging prostate cancer, which is identifying where the cancer is in the body using new imaging techniques like MRIs and PET scans. And this is going to help us select patients for the appropriate treatment or avoid treatments that are ultimately going to be futile in some patients.
There’s a lot of interest in the role of genetics in prostate cancer, both in the screening world and treatment. This is right now probably more important for patients with advanced disease getting medical treatment for advanced metastatic prostate cancer. But I think we’re learning more and more about the role of genetics in cancer and also learning about who doesn’t need aggressive treatment.
We’re kind of continuing to push the envelope about which patients can be safely watched. And initially, it was just the patients with a tiny amount of low-grade cancer were the only candidates for surveillance. And then people started to include patients with a moderate amount of low-grade cancer, and now even patients with small amounts of grade two cancer or intermediate risk cancers that traditionally would not have been considered for surveillance.
So some of these genetic and genomic tests are probably arguably useful in helping us identifying the higher risk patients who need treatment versus the lower-risk patients who may be able to be watched. And that’s something that will continue to evolve over time.
Ed Randall: Finally, thanks to both of you for taking time to be with us today and for putting up with questions from a Fordham University graduate who studiously avoided the Dean’s list and didn’t even take a science course in college unless you count geology.
Given that I have left at least two questions on the table. I invite you, Chad and you, Chris, to ask those questions of each other. Chris, what is a question about anything at all that you would like to ask Chad?
Dr. Christopher Anderson: Right. I’ll take this a little bit out of the clinical realm for a second. So you’ve heard about Chad. He’s an incredibly accomplished doctor, he wears a lot of hats: teacher, surgeon, liaison to cancer committees. He’s a father and a husband. Lot of spinning plates.
So tell us Chad, how do you manage to keep all these things balanced and have time for yourself and for your children and family while being so successful at work?
Dr. Chad Ritch: The short answer is I’m not sure. I just do it. I try my best. But honestly, I give a lot of credit to my wife. She’s a person that probably keeps everything in the house balanced. And she’s a surgeon too. She’s a gynecologist. But with her and being able to share the responsibility for a lot of things around the house, it gives me time to do things like what I’m doing right now.
And then when it comes time to relax and do things with the family, she’s great at organizing those things. So it’s important to have a good family and a good support system. And then colleagues. Like my partners that I work with here, I have great colleagues like you that I bounce ideas off regularly. And when I’m not sure about something I’m never afraid to ask. And they’re very supportive about my career and the things I want to do. So I think having good family support and colleagues is important to be able to do what we do every day.
Ed Randall: And Chad, what is a question—and every subject’s in play by the way—that you would want to ask Chris.
Dr. Chad Ritch: First question is what’s the temperature in New York right now?
Dr. Christopher Anderson: That’s 25 degrees.
Dr. Chad Ritch: Good. And the follow-up question to that is when are you coming to Miami?
Dr. Christopher Anderson: I can’t wait. I’d love to get down there. We’re freezing our butts off here.
Dr. Chad Ritch: There you go. That’s the invitation. That was the question. That’s all I wanted to hear. I’ll see you in a couple of weeks.
Dr. Christopher Anderson: Done. Buying my ticket.
Ed Randall: Chad, you don’t want to know the wind chill. And with that, we’ve reached the end of today’s Stay in the Game Podcast. Our guests have been Dr. Chad Ritch, part of the Medical School Faculty and a Urologic Oncologist in the University of Miami’s Health System and Dr. Christopher Anderson, an Assistant Professor, physician and researcher at the New York-Presbyterian/Columbia University Irving Medical Center in New York City.
Thank you again to both of you for sharing your time and your insights with us today. We are so honored to have you both. Thank you and the best of luck to both of you.
Dr. Christopher Anderson: Thanks, Ed.
Dr. Chad Ritch: Thanks, Ed.
Ed Randall: And thank you everybody for listening to our Stay in the Game Podcast. I’m Ed Randall.
Thanks for listening to the show. You can find program notes and a full transcript at the charity’s website, fansforthecure.org. Be sure to subscribe to our podcast in iTunes, Spotify, Stitcher, and everywhere good podcasts are available. And if you like what you heard, a positive review on iTunes will help other people also find our show.

